Connect With Us
Blog

Types of Neuropathy and Its Impact on Feet

Peripheral neuropathy is a condition caused by damage to the peripheral nerves, often resulting in numbness, tingling, burning sensations, and pain in the extremities. There are several types of peripheral neuropathy, each with its own set of causes and symptoms. Regardless of the underlying cause, peripheral neuropathy can have a significant impact on the feet, leading to decreased sensation, balance issues, and an increased risk of foot injuries and ulcers. Diabetic neuropathy is one of the most common types and is caused by nerve damage from prolonged exposure to high blood sugar levels in people with diabetes. Other types include compressive neuropathy, which occurs when nerves are compressed or pinched, and toxic neuropathy, which can result from exposure to certain medications, chemicals, or toxins. Proper foot care, including regular inspections, supportive footwear, and maintaining good blood sugar levels for diabetes, is essential for managing symptoms and preventing complications associated with peripheral neuropathy. If your feet are affected with any of the above symptoms, it is strongly suggested that you meet with a podiatrist who can offer you effective methods to manage the type of neuropathy you have.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Use of Braces for Ankle Sprains

Braces and splints play a vital role in the management and rehabilitation of foot and ankle injuries, particularly ankle sprains. These supportive devices are designed to immobilize and protect the affected joint. They also help to reduce pain and swelling, which can accelerate the healing process. For acute ankle sprains, the use of a functional ankle brace has been shown to be more effective than immobilization or compression wraps. This is true not only in terms of enhancing functional outcomes but also in preventing future ankle sprains. However, it is essential to seek professional guidance from a podiatrist for a proper diagnosis and treatment plan tailored to the individual’s needs. A podiatrist can assess the severity of the injury and recommend the most suitable brace or splint, ensuring correct sizing, fit, and length of use. Selecting the wrong brace or splint or using it incorrectly may impede healing or even worsen the symptoms. Also, prolonged use of a brace without proper rehabilitation may lead to joint stiffness and muscle weakness, increasing the risk of further complications. If you have sustained an ankle sprain, it is suggested that you schedule an appointment with a podiatrist to ensure optimal recovery and prevent recurrent injuries.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Foot Pain Caused by Cycling

Foot pain while cycling can quickly turn a joyful bike ride into a struggle. Whether it's blisters, hot spots, or the burning discomfort of hot-foot, understanding the root causes of foot pain during a ride is essential for finding relief. Blisters often arise from the repetitive rubbing and pressure points caused by wearing ill-fitting shoes. Meanwhile, hot-foot, which is a fiery sensation in the ball of the foot, typically occurs during long or hot rides due to nerve compression from foot swelling. To address these issues, wearing stiff-soled cycling shoes can improve power transfer and reduce pressure. A proper shoe fit is also important to ensure a snug yet comfortable feel, especially as feet tend to swell during rides. Optimizing your bike setup by adjusting cleat positions and experimenting with different pedal platforms may further alleviate pressure points. Maintaining good foot hygiene, selecting appropriate socks, and choosing pedal platforms suited to your riding style can all contribute to a less painful cycling experience. However, if foot pain persists after a long bike ride, it is suggested that you schedule an appointment with a podiatrist for an exam and diagnosis.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact one of our podiatrists of Comprehensive Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Are Bunions Affecting Your Everyday Life?
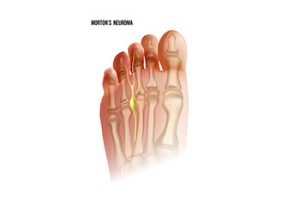
Morton’s Neuroma Is a Nerve Condition
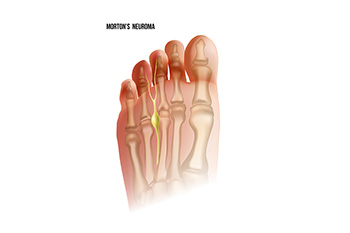
Morton's neuroma, a painful foot condition, stems from the compression of the plantar digital nerve, typically between the third and fourth toes. This nerve compression leads to the thickening of the nerve tissue, resulting in sharp, burning pain, tingling sensations, and numbness in the affected toes. Despite its name, Morton's neuroma is not a true neuroma, or tumor, but rather a nerve entrapment or irritation. The precise cause of Morton's neuroma remains unclear, though factors such as repetitive stress, wearing tight or high-heeled shoes, foot deformities, and certain activities that involve pressure on the forefoot are thought to contribute to its development. Diagnosis often involves a thorough examination by a podiatrist, including a physical assessment of the foot. This may include imaging tests like X-rays or MRI scans to confirm the condition. If you are experiencing pain in this part of your foot, it is suggested that you consult a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Comprehensive Foot & Ankle Center. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Early Onset Gout

Early onset gout, a form of inflammatory arthritis, can afflict individuals before the age of 40 typically manifesting as sudden and intense joint pain, commonly in the big toe. This condition arises due to the buildup of uric acid crystals in the joints, leading to inflammation and debilitating discomfort. Several risk factors contribute to the development of early onset gout, including genetics, a diet rich in purines found in red meat and seafood, alcohol consumption, and certain medical conditions like hypertension and hyperlipidemia. Elevated body mass index, or BMI also exacerbates the risk, as obesity often correlates with higher uric acid levels. If you are under 40 and believe you may be suffering from gout, it is strongly suggested that you include a podiatrist on your care team. This foot specialist can offer a range of interventions to alleviate pain and prevent future gout flare-ups.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.