Connect With Us
Blog

Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Recognizing the Symptoms of Flat Feet

Flat feet, or fallen arches, are a common condition where the arches of the feet collapse, causing the entire sole to touch the ground. Recognizing the symptoms of flat feet is essential for understanding and addressing this condition. One prevalent sign is pain or discomfort along the inner side of the ankle and arch. Individuals with flat feet may also experience swelling along the inside of the ankle. The lack of a visible arch when standing or walking is a visual indicator of flat feet. Overpronation, where the foot rolls inward excessively, can contribute to this condition and lead to related issues, including shin splints or knee pain. Fatigue and aching in the feet and legs can occur, especially after prolonged standing. If you have flat feet, it is suggested that you speak to a podiatrist who can provide you with effective relief options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Keep Your Feet Healthy So You Can Stay Active
Success of Ankle Replacement Surgery

There has been a growing interest in total ankle replacement due to concerns about the long-term results of ankle fusion surgery. This interest has led to the development of new ankle implants that better mimic the natural structure and movement of the ankle, including its ligaments and alignment. Although the newer 2nd-generation ankle replacements are showing promising results for patients with severe ankle arthritis, there are still challenges. One issue is that ankle replacements tend to fail more often than other joint replacements. This may be because it is hard for surgeons to perfectly replicate the ankle's complex stability and movement during surgery. To improve the chances of success, it is important to make sure this is the correct surgery for you. If you have not had success with more conservative treatments for ankle arthritis, it is suggested that you make an appointment with a podiatrist to see if you would be a good candidate for ankle replacement surgery.
In certain cases, in which the patient suffers from extreme pain or damage in a joint, joint replacement surgery may be deemed useful. If you have constant pain in a foot joint, consult with one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Joint Replacement Surgery?
Over time, joints wear down; this can be exacerbated by diseases and conditions. Joint replacement surgery, also known as arthroplasty, is when a damaged joint is surgically removed and replaced with a prosthesis. Prostheses, which can be made of ceramic, plastic, or metal, act as joints in lieu of an actual joint. One of the most prevalent causes for joint replacement is arthritis.
Arthritis in the Foot
Arthritis can occur in any joint in the body, including in the feet. Common types of arthritis in the foot are osteoarthritis, rheumatoid arthritis, and gout. The big toe is usually where arthritis occurs in the foot; this is known as hallux rigidus.
Joint Replacement Surgery in the Foot
The most common form of joint replacement in the foot is a first metatarsophalangeal (MTP) joint placement. MTP joint replacement surgery is designed to treat hallux rigidus. Surgery is not intensive, and recovery occurs within one to two months after the procedure has been done. Overall, joint replacement surgery is a safe and effective way to treat pain in the joint of the foot.
If you have any questions, please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Joint Replacement Surgery
When conservative, noninvasive treatments prove unsuccessful, podiatrists will often turn to surgery as the last line of treatment for their patients. If patients are suffering from joint pain, issues in mobility, or are seeking to correct a deformity, joint replacement surgery is an effective option. Joint replacement surgery is also successful in treating arthritis, which is the most common cause of improperly working joints.
Patients with symptoms that include joint pain, stiffness, limping, muscle weakness, limited motion, and swelling are typically considered for joint replacement surgery. Range of motion and activity post-surgery will vary between patients and depending on the specific surgery performed, the affected joint, and the damage that will need to be repaired.
Joint replacement surgery replaces the damaged cartilage and bone, the latter if required. The damaged cartilage is typically replaced with a prosthesis that is attached to the bone, allowing the implant to grow into the bone. Following surgery, the patient will typically undergo physical therapy to become familiar with movement using the replaced joint.
Foot Complications Linked to Diabetes

Diabetes is a chronic condition that affects how your body processes glucose. While it primarily impacts blood sugar levels, it can also lead to various health complications, including those related to the feet. Diabetes-related foot problems are a serious concern that can result from uncontrolled blood sugar levels over time. One common issue is neuropathy, where prolonged high blood sugar damages nerves, possibly leading to numbness, tingling, or foot pain. This sensory loss can make it difficult to notice injuries or ulcers. Another complication is poor circulation, which can slow down the body's ability to heal. Inadequate blood flow can lead to slow wound healing and increase the risk of infections. Diabetes can also cause changes in foot structure which may lead to issues such as bunions, hammertoes, and Charcot foot, a condition characterized by weakened bones and joints. Preventing diabetes-related foot problems involves maintaining good blood sugar control and regular foot care, in addition to choosing appropriate footwear. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you address and prevent foot complications.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
How Foot Bones Work Together in Unison
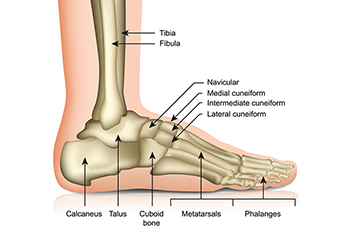
The human foot is a marvel of engineering, with a complex network of 26 bones working seamlessly in unison to support our body weight and enable a wide range of movements. These bones can be categorized into three main groups, known as the tarsal bones in the ankle, metatarsals in the arch, and phalanges in the toes. Tarsal bones provide the foot's stability and shock-absorbing capacity. They bear the weight and help transmit the forces generated during activities. Metatarsals form the foot's longitudinal arch, creating a flexible structure that acts as a lever during walking, running, and jumping. The phalanges, or toes, contribute to balance and provide dexterity. The biomechanics of the feet rely on an extensive network of muscles, tendons, and ligaments. Together, they allow for precise and controlled movements. When all components function harmoniously, the foot operates efficiently, ensuring that we can walk, run, and stand with stability and grace. Understanding this collaboration among foot bones highlights the importance of proper foot care and maintenance for a lifetime of healthy and pain-free mobility. If you would like additional information about the intricacies of the feet, it is suggested that you consult a podiatrist who can provide you with the information you are seeking.
If you have any concerns about your feet, contact one of our podiatrists from Comprehensive Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Lehigh Ave and Nazareth Hospital in Philadelphia, Collegeville Darby, and Langhorne, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Importance of Biomechanics in Podiatry
Biomechanics and its related study deal with the forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
Biomechanics and its related study deal with forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
The history of studying biomechanics dates back to ancient Egypt at around 3000 B.C., where evidence of professional foot care has been recorded. Throughout the centuries, advances in technology, science, and an understanding of the human body led to more accurate diagnosis of conditions such as corns for example. In 1974, biomechanics garnered a large audience when Merton Root founded Root Lab to make custom orthotics. He proposed that corrections of certain conditions could be implemented to gain strength and coordination in the area. Due to his research, we still use his basic principle of foot orthotics to this day.
As technology has improved, so have the therapeutic processes that allow us to correct deficiencies in our natural biomechanics. Computers can now provide accurate readings of the forces, movements, and patterns of the foot and lower leg. Critical treatment options can be provided to patients now who suffer from problems that cause their biomechanics to not function naturally. The best results are now possible thanks to 3D modeling and computing technologies that can take readings and also map out what treatment will do to the affected areas.
These advanced corrective methods were able to come to light thanks to an increase in both the technologies surrounding biomechanics and also the knowledge of how they work naturally. For example, shoe orthotics are able to treat walking inabilities by realigning the posture deviations in patients caused by hip or back problems. Understanding foot biomechanics can help improve movement and eliminate pain, stopping further stress to the foot. Speak with your podiatrist if you have any of these problems.